Asthma
Episodes
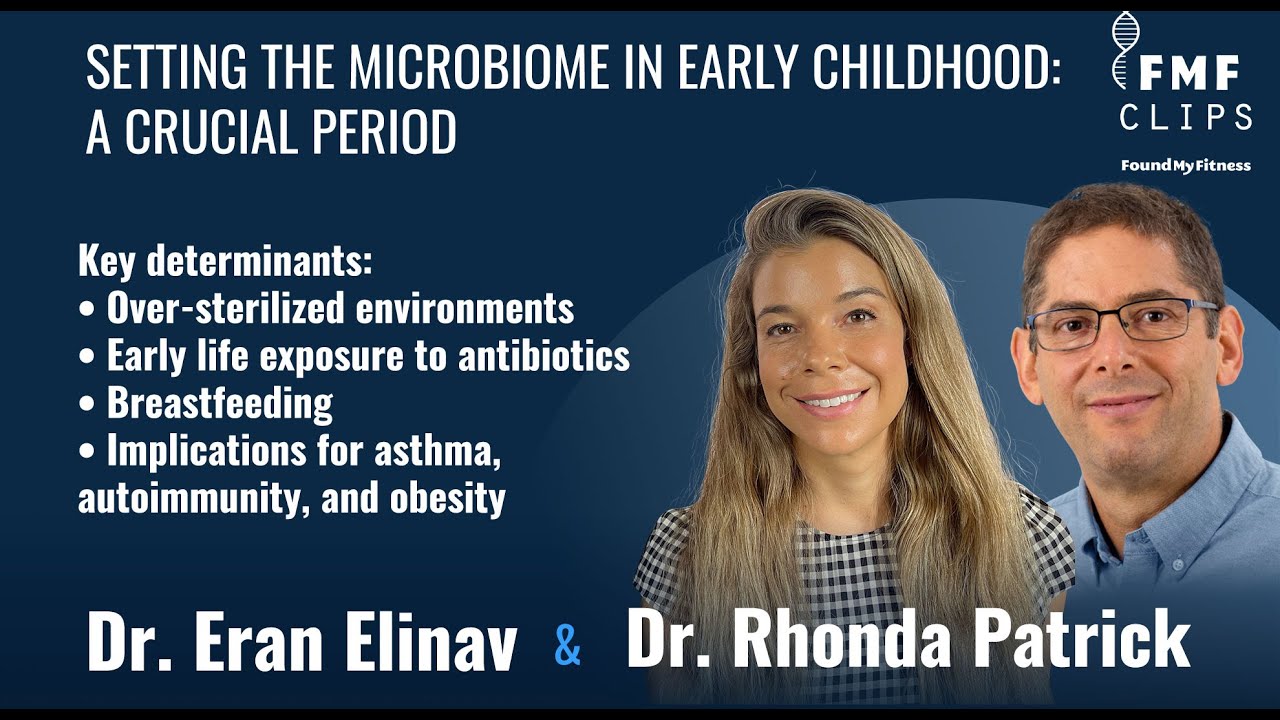
In this clip, Dr. Eran Elinav discusses the importance of the early childhood period in shaping a healthy microbiome.
Drs. Jed Fahey and Rhonda Patrick discuss concerns about the safety and efficacy of probiotic supplements.
-
In this clip, Dr. Eran Elinav discusses the importance of the early childhood period in shaping a healthy microbiome.
-
Drs. Jed Fahey and Rhonda Patrick discuss concerns about the safety and efficacy of probiotic supplements.
Topic Pages
News & Publications
-
Regular exercise during pregnancy may cut the risk of asthma in children by half by improving prenatal lung development. pubmed.ncbi.nlm.nih.gov
Asthma affects millions of children, and finding ways to prevent it before birth could be a game-changer. Some evidence suggests that physical activity during pregnancy promotes fetal lung development, potentially reducing children’s asthma risk. A recent study found that the children of mothers who engaged in regular physical activity during pregnancy were nearly half as likely to develop asthma.
Researchers analyzed data from 963 mother-child pairs participating in the Kuopio Birth Cohort study. They gathered information on maternal physical activity during pregnancy, potential influencing factors, and asthma diagnoses in the children when they were between the ages of 5 and 7 years.
They found that the children of mothers who engaged in physical activity three or more times per week during pregnancy were 46% less likely to develop asthma. This relationship held steady even after adjusting for factors like the length of pregnancy, delivery method, maternal health conditions, and family environment.
These findings suggest that regular physical activity during pregnancy could effectively reduce asthma risk in children. Experts recommend that pregnant women aim for about 150 minutes of moderate-intensity exercise every week. Learn about other healthy lifestyle practices for pregnancy in Aliquot #100: Optimizing for a Healthy Pregnancy and Early Childhood.
-
Testosterone protects men from developing allergic asthma by inhibiting a certain type of immune cell, mouse study suggests. (2017) www.sciencedaily.com
From the article:
“There is a very interesting clinical observation that women are more affected and develop more severe asthma than men, and so we tried to understand why this was happening,” Dr Seillet said.
“Our research shows that high levels of testosterone in males protect them against the development of allergic asthma. We identified that testosterone is a potent inhibitor of innate lymphoid cells, a newly-described immune cell that has been associated with the initiation of asthma.”
The research team found that innate lymphoid cells – or ILC2s – ‘sensed’ testosterone and responded by halting production of the cells.
“Testosterone directly acts on ILC2s by inhibiting their proliferation,” Dr Seillet said. “So in males, you have less ILC2s in the lungs and this directly correlates with the reduced severity of asthma.”
ILC2s are found in the lungs, skin and other organs. These cells produce inflammatory proteins that can cause lung inflammation and damage in response to common triggers for allergic asthma, such as pollen, dust mites, cigarette smoke and pet hair.
-
Eating fish rich in omega-3 fatty acids reduces risk of asthma in some children. www.sciencedaily.com
Asthma is a respiratory condition characterized by narrowed airways and difficulty breathing. It commonly manifests in early childhood and affects more than 339 million people worldwide. Findings from a new study suggest that dietary intake of omega-3 fatty acids among children who carry a common variant in the fatty acid desaturase gene reduces the risk of developing asthma.
Fatty acid desaturase is an enzyme that drives the biosynthesis of mono- and polyunsaturated fatty acids in the body. Impairments in the expression and activity of fatty acid desaturases drives many pathological conditions.
The authors of the study analyzed data from healthy male and female children enrolled in the Avon Longitudinal Study of Parents and Children, a prospective birth cohort study conducted in England. They assessed dietary intake of omega-3 fatty acids from fish via food frequency questionnaires when the children were 7 years old and collected information about the incidence of asthma among the children when they were 11 and 14 years of age. They replicated their analysis in the Swedish BAMSE birth cohort.
The authors of the study found no links between intake of omega-3 fatty acids from fish and the incidence of asthma in the full group of children. But when they looked at the subset of children who carried a variant in the fatty acid desaturase gene, they found that high intake of omega-3 fatty acids from fish reduced the risk of developing asthma 51 percent. These findings were replicated in the BAMSE cohort.
These findings suggest that dietary intake of fish rich in omega-3 fatty acids during childhood reduces the risk of developing asthma among children who carry a genetic variant of an enzyme involved in fatty acid synthesis. The authors of the study cautioned that their study was observational and did not identify any causes to explain the relationship.
-
A pilot study to investigate the immune modulatory effects of fasting in steroid-naïve mild asthmatics www.ncbi.nlm.nih.gov
A fasting mimetic diet blunts inflammation and intermittent fasting has shown ameliorative effects in obese asthmatics. To examine whether canonical inflammatory pathways linked with asthma are modulated by fasting we designed a pilot study in mild asthmatic subjects to assess the effect of fasting on: the NLRP3 inflammasome; Th2 cell activation and airway epithelial cell cytokine production. Subjects with documented reversible airway obstruction and stable mild asthma were recruited into this study where pulmonary function testing (PFT) and peripheral blood mononuclear cells (PBMCs) extraction was performed 24 hours after fasting, with repeated PFT-testing and blood draw 2.5 hours after refeeding. PFT’s were not changed by a prolonged fast. However, steroid-naïve mild asthmatics showed fasting-dependent blunting of the NLRP3 inflammasome. Furthermore, PBMCs from these fasted asthmatics co-cultured with human epithelial cells resulted in blunting of house dust mite-induced epithelial cell cytokine production, and reduced CD4+ T cell Th2 activation compared to refed samples. This pilot study shows that prolonged fasting blunts the NLRP3 inflammasome and Th2 cell activation in steroid-naïve asthmatics, as well as diminishes airway epithelial cell cytokine production. This identifies a potential role for nutrient-level dependent regulation of inflammation in asthma. Our findings support the evaluation of this concept in a larger study, as well as the potential development of caloric restriction interventions for the treatment of asthma.
-
Evidence suggests vitamin C substantially reduces bronchoconstriction caused by exercise www.sciencedaily.com
Exercise-induced bronchoconstriction – a narrowing of the airways in response to exercise – occurs in as much as 10 percent of the general population and up to 50 percent in some fields of competitive athletics. Findings from a meta-analysis suggest that vitamin C might reduce the incidence of exercise-induced bronchoconstriction.
Previous research demonstrated that vitamin C can triple respiratory tissue levels within an hour or two of a single oral dose of 1 or 2 grams. This local increase in vitamin C concentration appears to protect against acute increases in airway oxidative stress. In addition, vitamin C inhibits the production of prostaglandins and leukotrienes, biological compounds that participate in the pathogenesis of exercise-induced bronchoconstriction.
In addition, vitamin C halved the incidence of the common cold among people experiencing heavy short-term physical stress – an indication that vitamin C might also have other effects on people experiencing heavy physical exertion.
The authors of the current conducted analyses of nine studies that investigated varied aspects of the effects of vitamin C on exercise-induced bronchoconstriction. Three placebo-controlled studies analyzed the relative exercise-induced decline in forced expiratory volume, or FEV1, (a measure of respiratory capacity) with or without a vitamin C. They found that doses ranging between 0.5 and 2 grams of vitamin C reduced FEV1 decline by half. Similarly, five studies investigated the effects of vitamin C supplementation on respiratory symptoms after short-term heavy physical work and found that incidence was halved. One study investigated the duration of respiratory symptoms in young male swimmers and also found that incidence was halved.
The authors noted that a variety of factors might influence whether and to what degree vitamin C affects respiratory function during exercise, including the type of activity and the conditions under which it is performed, among others.